This page may contain affiliate links. If you make a purchase through any of these links I will make a small commission. As an Amazon Associate I earn from qualifying purchases.
When Dementia Patients Stop Eating and Drinking
Introduction
One of the most distressing developments in people with dementia is when they slowly stop eating and drinking.
Though it’s a natural part of the progression of the disease, there are several things you can do to try and halt its progress and help your loved one enjoy mealtimes and stay healthy for as long as possible.
Reasons Why Your Loved One Has Stopped Eating and Drinking
There are many reasons why a person with dementia may lose interest in or turn down, food, and drink.
- Depression: A common sign of depression is a loss of appetite, and depression is common in people with dementia. If your loved one has depression, then their appetite should improve if their depression is treated appropriately.
- Communication: As dementia progresses, people with dementia have difficulty communicating their needs – including the need that they are hungry or don’t like the food they have been given.
Alternative methods of communication and speech therapy to help your loved one express themselves better is often the solution for poor eating and drinking-related to communication difficulties.
- Pain: We’ve all experienced a bad toothache or sore throat. Your loved one may be having problems with their dentures, teeth, or gums. If they have difficulty communicating, then they won’t be able to tell you they’re experiencing pain.
Oral hygiene and regular mouth checks are essential to prevent oral pain and discomfort.
- Tiredness: If your loved one is fatigued, then they may stop eating partway through a meal or simply not eat at all. This can also cause concentration and coordination difficulties, so it’s best for your loved one to eat while they’re most alert.
- Medication: People react to medicine differently, and changes in brand or dose can result in appetite changes. Monitor your loved one carefully and speak to their doctor if you have any concerns.
- Physical Activity: Being active increases appetite, so if your loved one spends most of their day inactive, then it makes sense that they won’t have much of an appetite.
Encourage and assist them to be more active to increase their appetite and enhance their overall well-being.
- Constipation: This is a prevalent problem in patients with dementia, and the bloated and nauseous feeling that constipation creates makes them less likely to want to eat.
Encourage activity, fiber-rich foods, and drinking lots of liquids to help prevent constipation, and speak to your loved one’s doctor if the problem persists.
Health Concerns
While weight loss isn’t concerning to the average person, it can be quite concerning when it affects someone with dementia. This is because weight loss can affect the immune system and make it harder for your loved one with dementia to fight infections and other illnesses.
Extreme weight loss can also increase their risk of falling, making it more difficult for them to retain their independence, and create other physical health problems like:
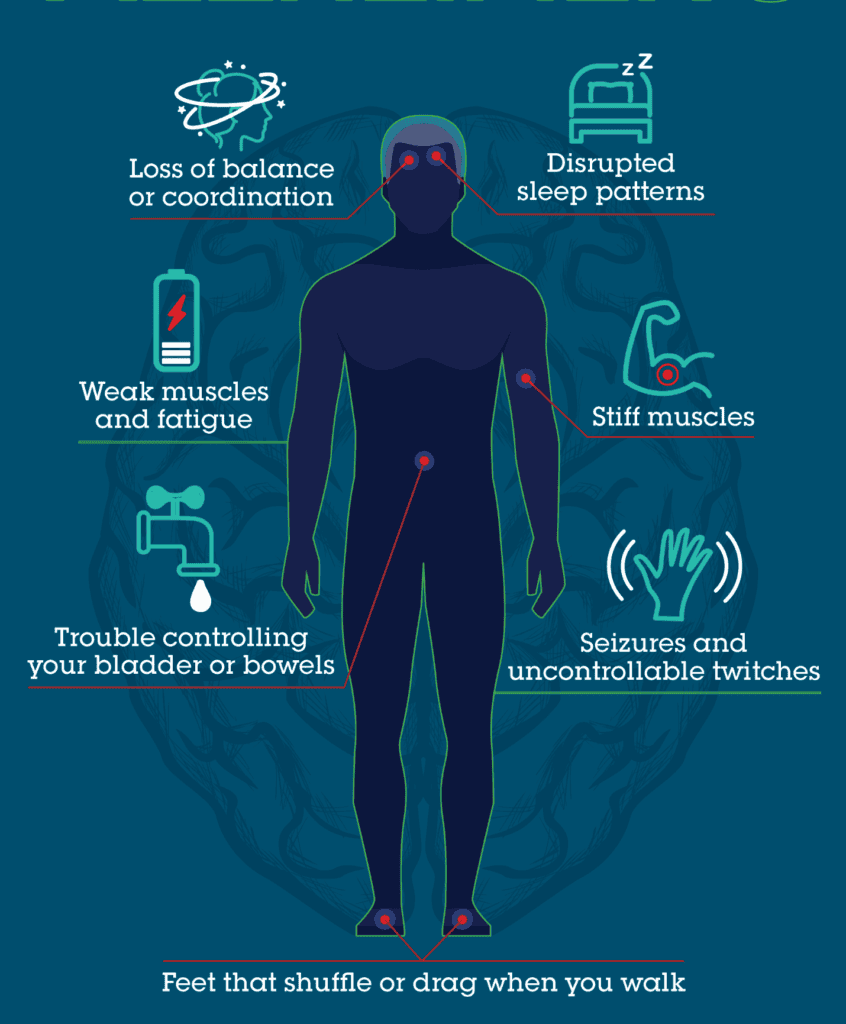
Image courtesy of WebMD
If your loved one develops severe swallowing and/or chewing difficulties (known as dysphagia), then they become at risk for choking and infection. Delirium and severe dehydration can also occur as a result of inadequate nutritional intake and extreme weight loss.
How You Can Help Your Loved One Eat and Drink
There are several ways that you can try and increase your loved one’s appetite and interest in food and drink.
You know your loved one, their preferences, and their routines best, and that puts you at an automatic advantage. You also know their likes and dislikes and what they can physically manage when it comes to eating and drinking.
Here are some ideas to help encourage your loved one’s appetite:
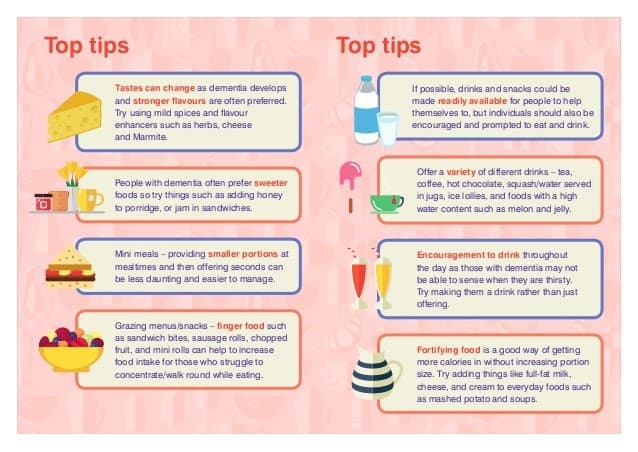
Image courtesy of WessexAHSN
- Make food look and smell appealing. I find that using different tastes, colors, smells, and textures really help my Grandpa want to eat, especially if he’s in the kitchen and can see and smell the food being prepared.
- Look for opportunities to encourage your loved one to eat. My Grandpa is most alert and willing to engage in the mornings, so I take advantage of this by making him a big breakfast with a high-calorie count.
I still encourage him to eat throughout the day, but I find that the morning boost helps him quite a bit.
- Give them the food they like. Even if it seems like it’s much of the same thing, giving my Grandpa small, regular portions of food that he enjoys works far better than a heaping plate of food that he’s indifferent towards.
- Keep trying different types of food and drinks: Sometimes, the foods your loved one used to love most now become the ones they can’t stand and vice versa.
I’ve found that trying out different smoothies and milkshakes work well with my Grandpa, and they always seem to bring a smile to his face. The truth is that your loved one’s food tastes may change, so try more robust flavors and sweeter foods if possible.
- Let them eat their dessert, even if they haven’t had their main. People with dementia often prefer sweet foods over savory foods. While it’s essential for them to have a balanced diet, it’s also essential that they enjoy their meals and actually eat something.
While not ideal, only eating dessert is better than eating absolutely nothing at all.
- Make sure their food stays warm. No one enjoys eating cold soup or drinking a lukewarm cup of tea. When food cools, it loses its appeal.
I’ve had to start serving my Grandpa half portions of his meals because it takes him a while to eat, and his food goes cold. While he’s eating the first half, I make sure I keep the other half warm using a plate warmer and the microwave.
- Soften their food if they have difficulties chewing and/or swallowing. You might have to consult with a dietician and/or speech therapist for this one.
My Grandpa enjoys soft foods like scrambled eggs, though I do know of some people with dementia who take pureed food but need help from a dietician to ensure that it’s nutritious and has enough flavor.
- Encourage your loved one to get involved in mealtimes. Sometimes, my Grandpa enjoys taking part in the actual cooking of the food or setting the table.
On the days where he doesn’t feel like get involved, I make sure he at least sits in the kitchen so he can be passively involved while I talk to him and keep him engaged. By doing this, I also use eating and drinking as social and activity opportunities for my Grandpa as well.
- Always give them encouragement and gentle reminders to eat. My Grandpa’s concentration has really deteriorated over the last couple of years, so I often have to remind him to continue eating or when it’s time to eat.
I always make sure I remind him in a calm and soothing voice while making sure that the environment is relaxed and friendly.
- Keep trying. It’s easy to get despondent when your loved one doesn’t cooperate with you, and eating and drinking becomes a chore. Try and aim for the least stressful situations and keep trying.
If your loved one continues to refuse food, then you should speak to their doctor and get some advice on the best way forward.
Tube Feeding
Known as Artificial Nutrition and Hydration (ANH), feeding tubes are usually only recommended and utilized in the later stages of a person’s dementia – when they are no longer able to chew or swallow at all and simply aren’t getting enough nutritional intake for survival.
The choice to use ANH is a difficult decision that families need to make along with the guidance of their loved one’s doctor. Inserting feeding tubes requires hospital admission, which can be very distressing to your loved one with dementia and increase the risk of infection at the site of insertion.
There are four main types of tube feeding, which include:
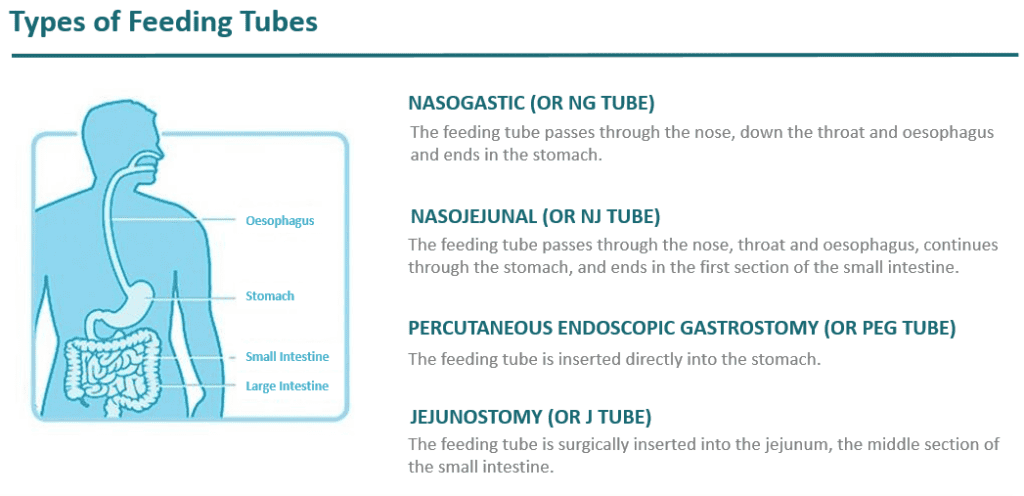
Image courtesy of Nestle Health Science
Though there are four main types of tube feeding, the two most common types are:
- Nasogastric Tube (NGT) Feeding: A thin tube that is passed through the nose down to the stomach. Liquid food is then passed through this tube into the stomach for digestion.
These tubes aren’t ideal for long-term use and can cause irritation in the nasal passages.
- Percutaneous Endoscopic Gastrostomy (PEG) Feeding: A thicker tube that is passed directly into the stomach through the stomach wall.
It is more comfortable than an NGT and can be left in place long-term. Sometimes, the PEG may cause infection and soreness around the tube site.
Conclusion
It can be very distressing when your loved one with dementia stops eating and drinking, and you may feel at a loss of what to do. However, it’s important to remember that there are many options available to you, and several healthcare professionals that are trained for this type of dementia care.
You aren’t alone in trying to ensure the best quality of life for your loved one, and you need only reach out to get the help that you need.
Thank you Howard for sharing the valuable information. This helps.
My dad is diagnosed with Vascular Dementia and we are going through similar situation.
Are there any common or known physiological or neurological causes for a Frontotemporal Dementia patient to stop eating?